Medical Software Development: Revolutionizing Healthcare
In today’s digital age, technology has permeated every aspect of our lives, including the healthcare industry. Medical software development has emerged as a game-changer, revolutionizing the way medical professionals operate and improving patient care.
The development of medical software has brought numerous benefits to the healthcare sector. One of the most notable advantages is improved efficiency and accuracy in patient care. With electronic health records (EHR) systems, medical professionals can easily access patient information, eliminating the need for manual paperwork and reducing errors caused by illegible handwriting or misplaced documents. This streamlined process allows doctors and nurses to spend more time focusing on patient care rather than administrative tasks.
Another significant aspect of medical software development is the integration of clinical decision support systems (CDSS). These intelligent systems provide healthcare providers with real-time guidance based on evidence-based medicine and clinical guidelines. CDSS not only assists in accurate diagnosis but also helps prevent medication errors and adverse drug interactions. By leveraging advanced algorithms and machine learning capabilities, CDSS enhances diagnostic accuracy and improves patient outcomes.
Telemedicine is another area where medical software development has made significant strides. Telemedicine platforms enable patients to consult with healthcare professionals remotely, eliminating geographical barriers and providing access to quality healthcare services for those in remote areas or with limited mobility. Through video consultations, patients can receive timely medical advice, prescriptions, or follow-up care without leaving their homes. This technology has become even more crucial during the COVID-19 pandemic when social distancing measures are in place.
Moreover, medical software development has facilitated research and innovation in the field of medicine. With data analytics tools integrated into these systems, researchers can analyze large volumes of patient data to identify patterns, trends, and potential breakthroughs in treatment options. This data-driven approach enables evidence-based medicine and fosters collaboration among researchers worldwide.
However, it is important to note that medical software development comes with its own set of challenges. Ensuring data security and privacy is of utmost importance, as healthcare systems deal with sensitive patient information. Developers must adhere to strict regulations and implement robust security measures to protect patient data from breaches or unauthorized access.
In conclusion, medical software development has transformed the healthcare industry, making it more efficient, accurate, and accessible. From electronic health records to clinical decision support systems and telemedicine platforms, technology has revolutionized the way medical professionals deliver care. As advancements continue to unfold, we can expect further improvements in patient outcomes and a brighter future for healthcare worldwide.
8 Frequently Asked Questions About Medical Software Development
- What is the process for developing medical software?
- What are the best practices for developing medical software?
- How can I ensure that my medical software meets regulatory standards?
- How do I ensure that my medical software is secure and compliant?
- What technologies should I use when developing medical software?
- How can I make sure my medical software is user-friendly and accessible to all users?
- How do I make sure that my medical software is reliable and efficient?
- What challenges should I be aware of when developing medical software?
What is the process for developing medical software?
The process for developing medical software involves several key steps to ensure the creation of a robust and reliable solution. Here is an overview of the typical process:
- Requirements Gathering: The first step is to gather requirements by collaborating with healthcare professionals, stakeholders, and end-users. This involves understanding their needs, workflows, and desired functionalities for the software.
- Planning and Design: Based on the gathered requirements, a detailed plan is created that outlines the project scope, timelines, resources needed, and technical specifications. The design phase involves creating wireframes or prototypes to visualize the user interface and overall system architecture.
- Development: The development phase involves coding and programming the software according to the design specifications. Developers follow best practices in coding standards, security protocols, and regulatory compliance specific to medical software.
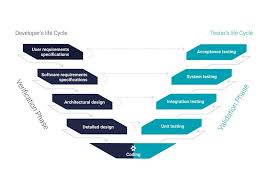
- Testing: Rigorous testing is crucial in medical software development to ensure functionality, performance, security, and compliance with industry standards (such as HIPAA). This includes unit testing, integration testing, system testing, usability testing, and validation against regulatory requirements.
- Regulatory Compliance: Medical software must adhere to strict regulations such as HIPAA (Health Insurance Portability and Accountability Act) or FDA guidelines (if applicable). Compliance documentation should be prepared throughout the development process to meet these regulations.
- Deployment: Once all necessary tests are successfully completed and regulatory compliance is met, the software can be deployed in a production environment or made available for distribution through app stores or other platforms.
- Maintenance and Updates: After deployment, ongoing maintenance is essential to address any bugs or issues that may arise post-launch. Regular updates are also required to add new features, improve performance/security, or comply with changing regulations.
Throughout the entire process of developing medical software, collaboration between developers, healthcare professionals, quality assurance teams, regulatory experts (if needed), and end-users is crucial for success. Effective communication ensures that all stakeholders’ requirements are met while maintaining the highest standards of quality, security, and compliance in the medical software.
What are the best practices for developing medical software?
Developing medical software requires adherence to stringent standards and best practices to ensure patient safety, data security, and regulatory compliance. Here are some essential best practices for developing medical software:
- Regulatory Compliance: Familiarize yourself with the relevant regulatory requirements, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or the Medical Device Regulation (MDR) in the European Union. Ensure that your software complies with these regulations to protect patient data and meet legal obligations.
- User-Centered Design: Prioritize user experience and usability when designing medical software. Involve healthcare professionals throughout the development process to understand their needs, workflows, and pain points. Conduct user testing and gather feedback to refine the interface, ensuring intuitive navigation and efficient use.
- Interoperability: Medical software should be designed to integrate seamlessly with existing healthcare systems, such as electronic health record (EHR) systems or laboratory information management systems (LIMS). Implement interoperability standards like Health Level 7 (HL7) or Fast Healthcare Interoperability Resources (FHIR) to facilitate data exchange between different platforms.
- Data Security and Privacy: Protecting patient data is paramount in medical software development. Follow industry-standard encryption protocols to secure sensitive information both during transmission and storage. Implement access controls, authentication mechanisms, audit logs, and regular security assessments to prevent unauthorized access or breaches.
- Testing and Validation: Rigorous testing is crucial in medical software development. Conduct comprehensive functional testing, performance testing, integration testing, and usability testing to ensure that your software performs reliably under various scenarios. Validate your software against relevant standards or guidelines specific to your target market or intended use.
- Documentation: Maintain comprehensive documentation throughout the development process. Document design decisions, system architecture, algorithms used, validation procedures performed, risk assessments conducted, and any other relevant information for future reference or regulatory audits.
- Quality Assurance: Establish a robust quality assurance process to ensure that your medical software meets the highest standards. Implement a formalized software development life cycle (SDLC) with defined milestones, code reviews, and continuous integration practices. Adhere to recognized quality management systems such as ISO 13485 for medical devices.
- Ongoing Maintenance and Support: Medical software requires regular updates and maintenance to address bugs, security vulnerabilities, and evolving regulatory requirements. Provide timely support to healthcare providers or end-users to address any issues or concerns promptly.
- Collaboration and Compliance with Standards: Collaborate with industry experts, healthcare professionals, and regulatory bodies to stay informed about emerging trends, guidelines, and best practices in medical software development. Engage in knowledge sharing activities and participate in relevant conferences or forums.
By following these best practices, you can develop reliable, secure, and compliant medical software that enhances patient care while meeting industry standards and regulatory requirements.
How can I ensure that my medical software meets regulatory standards?
Ensuring that your medical software meets regulatory standards is crucial to ensure patient safety and compliance with applicable laws. Here are some key steps to follow:
- Familiarize Yourself with Regulatory Requirements: Thoroughly research and understand the specific regulations that apply to medical software development in your target market. This may include regional regulations such as FDA regulations in the United States or EU Medical Device Regulations in Europe.
- Engage Regulatory Experts: Consider involving regulatory experts or consultants who specialize in medical software development. They can provide valuable guidance and help navigate the complex regulatory landscape, ensuring that your software meets all necessary requirements.
- Conduct Risk Assessment: Perform a comprehensive risk assessment of your software to identify potential hazards and risks associated with its use. This includes analyzing possible failure modes, assessing their impact on patient safety, and implementing risk mitigation strategies.
- Follow Software Development Standards: Adhere to recognized software development standards such as ISO 13485 or IEC 62304, which provide guidelines for quality management systems and software lifecycle processes specific to medical devices.
- Implement Design Controls: Establish design controls throughout the development process to ensure traceability, validation, verification, and documentation of all design activities. This includes requirements management, design inputs/outputs, testing protocols, and change control procedures.
- Document Software Validation: Conduct thorough validation of your medical software to demonstrate its effectiveness, accuracy, and reliability in meeting its intended purpose. Document all validation activities performed during the development process.
- Establish Quality Management System (QMS): Implement a robust QMS that complies with relevant quality standards such as ISO 9001 or ISO 13485. This system should cover all aspects of your organization’s operations related to medical software development.
- Perform Usability Testing: Conduct usability testing with intended users to ensure that your software is intuitive, user-friendly, and meets their needs effectively while minimizing the risk of errors or misuse.
- Maintain Vigilance: Establish post-market surveillance processes to monitor the performance, safety, and effectiveness of your medical software after it is released. Implement mechanisms for reporting and addressing any adverse events or incidents promptly.
- Stay Updated: Keep abreast of evolving regulatory requirements and industry best practices. Regularly review and update your software to ensure ongoing compliance with the latest standards and regulations.
Remember, compliance with regulatory standards is an ongoing commitment. Regular audits, assessments, and continuous improvement efforts are essential to maintain compliance throughout the lifecycle of your medical software.
How do I ensure that my medical software is secure and compliant?
Ensuring the security and compliance of medical software is crucial to protect sensitive patient data and maintain the trust of healthcare providers and patients. Here are some key steps to follow:
- Understand Regulatory Requirements: Familiarize yourself with the relevant regulations governing medical software, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, General Data Protection Regulation (GDPR) in Europe, or other regional laws specific to your location. Understand the specific requirements related to data privacy, security, and breach notification.
- Conduct Risk Assessments: Perform a thorough risk assessment to identify potential vulnerabilities in your software system. This includes assessing risks related to data storage, transmission, access controls, authentication mechanisms, and potential external threats. Identify areas where improvements are needed.
- Implement Strong Data Encryption: Ensure that all sensitive data is encrypted both at rest (stored) and in transit (during transmission). Encryption helps protect data from unauthorized access or interception. Use industry-standard encryption algorithms and secure protocols for communication.
- Establish Access Controls: Implement strict access controls to limit system access only to authorized individuals based on their roles and responsibilities. This includes strong password policies, multi-factor authentication (MFA), session timeouts, and regular user access reviews.
- Regularly Update Software: Keep your medical software up-to-date with the latest security patches and updates provided by vendors or developers. Regularly patching vulnerabilities helps prevent exploitation by malicious actors.
- Conduct Penetration Testing: Perform regular penetration testing on your software system to identify any weaknesses or vulnerabilities that could be exploited by hackers or unauthorized users. Engage ethical hackers who specialize in healthcare systems to simulate real-world attacks and provide recommendations for improvement.
- Train Staff on Security Practices: Provide comprehensive training for all personnel who have access to the medical software system. Educate them about best practices for data protection, secure password management, phishing awareness, and handling potential security incidents.
- Implement Data Backup and Disaster Recovery Plans: Establish a robust backup strategy to ensure that data can be restored in case of system failure, natural disasters, or cyber-attacks. Regularly test the restoration process to verify its effectiveness.
- Perform Regular Security Audits: Conduct periodic security audits to assess the compliance and effectiveness of your security measures. Engage third-party auditors who specialize in healthcare compliance to ensure adherence to regulatory requirements.
- Stay Informed: Stay updated on emerging security threats, industry best practices, and evolving regulatory requirements related to medical software development. Join relevant forums, attend conferences, and engage with industry experts to stay abreast of the latest developments.
By following these steps, you can significantly enhance the security and compliance of your medical software system, safeguard patient data, and maintain the trust of healthcare providers and patients alike.
What technologies should I use when developing medical software?
When developing medical software, it is crucial to choose the right technologies that meet the specific requirements of the project. Here are some key technologies commonly used in medical software development:
- Programming Languages: Depending on the type of application, programming languages like Java, C#, or Python are often used for backend development. JavaScript and its frameworks (such as React or Angular) are commonly employed for frontend development.
- Database Management Systems: Robust and secure database management systems (DBMS) are essential for storing and managing patient data. Popular choices include MySQL, PostgreSQL, or MongoDB.
- Cloud Computing: Leveraging cloud computing platforms like Amazon Web Services (AWS), Microsoft Azure, or Google Cloud can provide scalability, flexibility, and security for medical software applications.
- Health Level 7 (HL7): HL7 is a set of international standards for exchanging healthcare information electronically. Integrating HL7 protocols into your software allows seamless interoperability with other healthcare systems.
- Application Programming Interfaces (APIs): APIs enable integration with external systems such as electronic health record (EHR) systems or laboratory information management systems (LIMS). FHIR (Fast Healthcare Interoperability Resources) is a popular API standard in healthcare.
- Security Measures: Given the sensitive nature of patient data, implementing robust security measures is paramount. Technologies like encryption algorithms, secure socket layers (SSL), and two-factor authentication should be considered to ensure data privacy and protection.
- Machine Learning and Artificial Intelligence: These technologies can enhance medical software by enabling predictive analytics, image recognition, natural language processing, and automated decision-making capabilities.
- Mobile Development Frameworks: If you plan to develop mobile applications for healthcare professionals or patients, frameworks like React Native or Flutter can help you build cross-platform apps efficiently.
- Virtual Reality (VR) and Augmented Reality (AR): These emerging technologies have potential applications in medical training simulations or surgical planning, providing immersive and interactive experiences.
- Compliance and Regulations: Ensure that your software adheres to regulatory standards such as HIPAA (Health Insurance Portability and Accountability Act) or GDPR (General Data Protection Regulation) to maintain data privacy and legal compliance.
It’s important to note that the choice of technologies should align with the specific requirements, scalability needs, budget, and timeline of your medical software project. Consulting with experienced developers or technology experts in the healthcare industry can help you make informed decisions.
How can I make sure my medical software is user-friendly and accessible to all users?
Ensuring that your medical software is user-friendly and accessible to all users is crucial for providing a positive user experience and inclusive healthcare services. Here are some key considerations to make your medical software more user-friendly and accessible:
- User-Centered Design: Adopt a user-centered design approach by involving end-users, such as healthcare professionals and patients, throughout the development process. Conduct usability testing and gather feedback to understand their needs, preferences, and pain points. Incorporate their input into the software’s design and functionality.
- Intuitive Interface: Design a clean and intuitive user interface (UI) that is easy to navigate. Use clear labels, logical workflows, and familiar icons to guide users through the software. Minimize clutter and ensure that essential information is prominently displayed.
- Consistent Layout: Maintain consistency in the layout of menus, buttons, and navigation across different screens/pages of your software. This consistency helps users quickly learn how to interact with the system and reduces cognitive load.
- Accessibility Standards: Follow accessibility standards such as the Web Content Accessibility Guidelines (WCAG) to ensure that your software can be used by individuals with disabilities. Provide options for adjusting text size, color contrast, and support keyboard navigation for those who cannot use a mouse.
- Multilingual Support: Consider incorporating multilingual support into your software so that users can access it in their preferred language. This is particularly important in diverse healthcare settings where patients may have limited English proficiency.
- Clear Instructions & Help Documentation: Include clear instructions within the software itself to guide users on how to perform various tasks or access specific features. Additionally, provide comprehensive help documentation or tutorials that users can refer to when needed.
- Training & Support: Offer training sessions or workshops for healthcare professionals who will be using your software regularly. Provide ongoing technical support channels such as email, chatbots, or phone assistance to address any issues or questions that users may have.
- Regular Updates & User Feedback: Continuously improve your software based on user feedback and changing needs. Regularly release updates that address bug fixes, enhance usability, and introduce new features. Encourage users to provide feedback and actively listen to their suggestions for improvement.
- Security & Privacy: Ensure that your software complies with relevant security and privacy regulations, such as HIPAA (Health Insurance Portability and Accountability Act). Protect patient data through encryption, secure authentication, access controls, and regular security audits.
By prioritizing user-friendliness and accessibility in the development of your medical software, you can enhance user satisfaction, promote inclusivity, and ultimately deliver better healthcare experiences for all users.
How do I make sure that my medical software is reliable and efficient?
Ensuring the reliability and efficiency of medical software is crucial to provide quality healthcare services and maintain patient safety. Here are some key considerations to help you achieve that:
- Requirements Gathering: Clearly define the requirements of your medical software in collaboration with healthcare professionals, clinicians, and end-users. Understand their needs, workflows, and pain points to develop a solution that addresses their specific requirements.
- User-Centric Design: Design the software with a user-centric approach, keeping the end-users in mind. The interface should be intuitive, user-friendly, and easy to navigate. Conduct usability testing and gather feedback from potential users to refine the design.
- Compliance with Regulations: Ensure that your medical software complies with relevant regulatory standards such as HIPAA (Health Insurance Portability and Accountability Act) in the United States or GDPR (General Data Protection Regulation) in Europe. Adhering to these regulations ensures patient data privacy and security.
- Robust Testing: Implement comprehensive testing methodologies throughout the development process. Conduct functional testing to verify that all features work as intended. Perform performance testing to assess its speed, scalability, and stability under various conditions.
- Security Measures: Implement stringent security measures to protect patient data from unauthorized access or breaches. Use encryption techniques for data transmission and storage, employ secure authentication methods, and regularly update security patches.
- Interoperability: Ensure that your medical software can seamlessly integrate with other healthcare systems such as electronic health record (EHR) systems or laboratory information systems (LIS). Interoperability allows for efficient exchange of information between different systems, improving workflow efficiency.
- Continuous Improvement: Software development is an ongoing process; therefore, strive for continuous improvement through regular updates and enhancements based on user feedback and changing industry needs.
- Training and Support: Provide comprehensive training programs for users to ensure they can effectively utilize the software’s features. Additionally, establish a dedicated support system to address any issues or concerns promptly.
- Collaboration with Healthcare Professionals: Involve healthcare professionals throughout the development process to gain valuable insights and feedback. Their expertise and input can help refine the software and ensure it meets the needs of the medical community.
- Post-Deployment Monitoring: Continuously monitor the performance and usage of your medical software after deployment. Collect user feedback, track system performance metrics, and address any reported issues promptly to maintain reliability and efficiency.
By following these guidelines, you can enhance the reliability and efficiency of your medical software, ultimately improving patient care and outcomes.
What challenges should I be aware of when developing medical software?
When developing medical software, it is crucial to be aware of the following challenges:
- Regulatory Compliance: The healthcare industry is heavily regulated to ensure patient safety and data privacy. Developers must navigate complex regulations such as HIPAA (Health Insurance Portability and Accountability Act) in the United States or GDPR (General Data Protection Regulation) in the European Union. Compliance with these regulations is essential to avoid legal issues and maintain patient trust.
- Data Security and Privacy: Medical software deals with sensitive patient data, including personal information and health records. Ensuring robust security measures, such as encryption, access controls, and secure data storage, is vital to protect against data breaches or unauthorized access. Compliance with privacy regulations is crucial for maintaining patient confidentiality.
- Interoperability: In the healthcare ecosystem, various software systems need to exchange information seamlessly. Achieving interoperability between different medical software applications can be challenging due to varying standards, protocols, and technologies used by different vendors. Ensuring compatibility and smooth data exchange between systems enhances efficiency and improves patient care.
- Usability and User Experience: Medical software should be intuitive and user-friendly for healthcare professionals who use it daily. Designing interfaces that are easy to navigate, understand, and operate is crucial for efficient workflow management. Conducting usability testing with end-users during development can help identify potential usability issues early on.
- Integration with Legacy Systems: Many healthcare organizations still rely on legacy systems that may not be easily compatible with modern medical software solutions. Integrating new software with existing infrastructure can present technical challenges that need to be addressed during development to ensure seamless operation across all systems.
- Scalability: Healthcare facilities handle vast amounts of data that continue to grow over time. Medical software should be designed with scalability in mind to accommodate increasing data volumes without compromising performance or functionality.
- Testing and Validation: Thorough testing of medical software is essential to ensure its reliability, accuracy, and safety. Rigorous validation processes, including testing for functionality, interoperability, security, and regulatory compliance, should be conducted to identify and address any potential issues or vulnerabilities.
- User Training and Support: Adequate training and ongoing support for healthcare professionals using the software are critical for successful implementation. Providing comprehensive documentation, training materials, and responsive customer support can help users navigate the software effectively and address any issues that may arise.
By being aware of these challenges and addressing them proactively during the development process, you can create robust and reliable medical software that meets regulatory requirements, protects patient data, enhances user experience, and improves overall healthcare outcomes.